Life Cycle & Transmission
Did you know?
“Flavus” is Latin for “yellow.” Flaviviruses are actually named after the yellow fever virus, which causes jaundice, or yellowing of the skin.
Powassan virus (POWV), also known as deer tick virus, is spread to humans by the bite of an infected tick (Ixodes scapularis). POWV is a type of arbovirus, meaning it can be transmitted by arthropods, such as ticks. More specifically, it is a flavivirus, meaning it belongs to the family Flaviviridae. These are single-stranded RNA viruses that replicate in the cytoplasm of host cells. Unlike other tick-borne diseases, Powassan has a much shorter transmission time, as infection can occur within 15 minutes after tick attachment (Ebel and Kramer 2004). For more information on disease transmission and the life cycle of deer ticks, please see the “Tick Ecology” section.
Computer illustration of Powassan virus particles.
Who Gets Powassan Virus & Where?
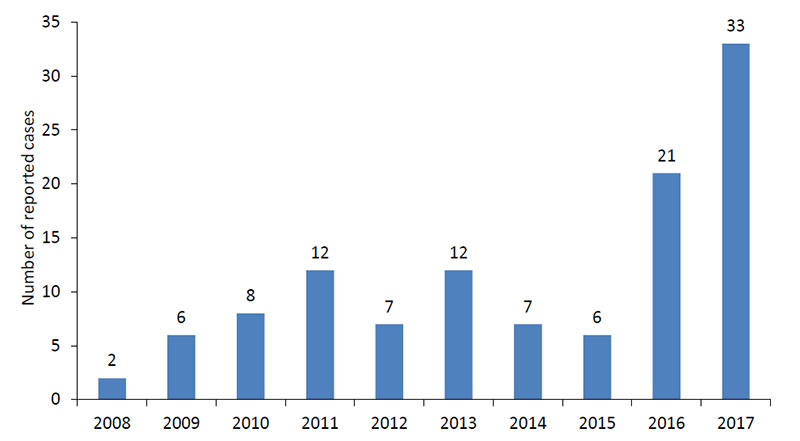
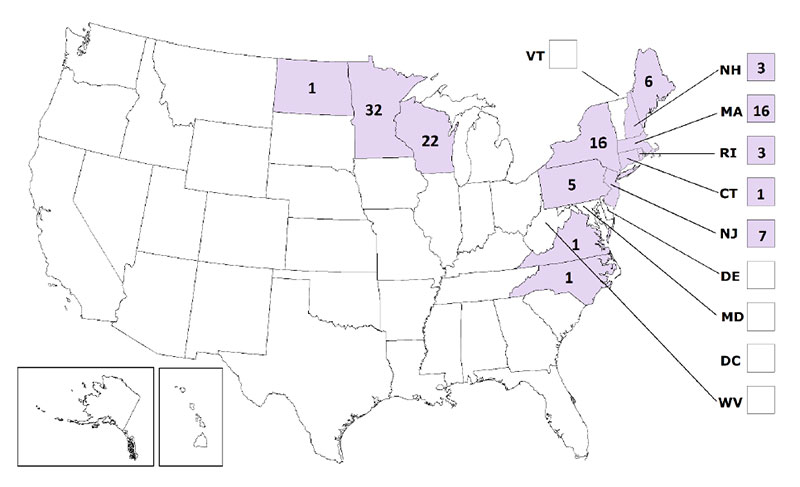
Powassan virus was named after the town of Powassan, Ontario, where it was isolated in 1958 in a young boy who died from encephalitis. However, the first reported case of Powassan virus in Wisconsin did not occur until 2003 (Johnson et al 2010). In the U.S., Powassan virus has been reported primarily in the Northeast and the Great Lakes region. These cases occur most frequently in late spring/early summer, when nymphs are most active. People who engage in outdoor work and recreational activities in endemic regions are more likely to be infected.
Symptoms
Many people who become infected with POWV do not develop symptoms. However, symptoms can appear between 1 week-1 month after a tick bite, and include:
Encephalitis (inflammation of the brain)
Meningitis (inflammation of the membranes surrounding the brain and spinal cord)
Fever, headache, vomiting
Weakness and confusion
Loss of coordination
Speech difficulties
Seizures
Diagnosis
Diagnosis of Powassan virus involves imaging evidence, such as a computed tomography (CT) scan or magnetic resonance imaging (MRI), to look for brain abnormalities. Blood tests that detect antibodies against POWV are also needed to confirm a diagnosis (CDC 2018). In fact, diagnosis of Powassan virus is largely serologic, as Powassan virus or Powassan virus nucleic acid is often difficult to isolate in clinical samples.
Treatment
There are currently no medications to treat or prevent Powassan virus. People with severe POWV often need to be hospitalized. Their treatment may include respiratory support, intravenous fluids, and medications to reduce swelling in the brain (CDC 2018).
For information on prevention, please see the “Tick Ecology” section.
Sources
Ebel and Kramer 2004. (“Short report: duration of tick attachment required for transmission of Powassan virus by deer ticks”): https://www.researchgate.net/publication/8332784_Short_report_Duration_of_tick_attachment_required_for_transmission_of_Powassan_virus_by_deer_ticks
Johnson et al 2010. (“Tickborne Powassan Virus infections Among Wisconsin Residents”): http://www.wisconsinmedicalsociety.org/_WMS/publications/wmj/pdf/109/2/91.pdf
CDC 2018 (“Powassan Virus”): https://www.cdc.gov/powassan/index.html
For additional reading, please visit the “Resources” tab.